“Detoxing” Requires Guts!
by Ashley Koff
Nutrition
Good food and hydration, plus the human body’s built-in detox brilliance, promote the optimal digestion and absorption at the core of your clients’ nutritional fitness.
 Attempting to inspire better eating habits, nutrition educators have long told people, “You are what you eat,” with the notion that “being” broccoli is more compelling than “being” a double cheeseburger or a supersized beverage. Yet, as we observe the global obesity epidemic and the dietary challenges we see daily with clients, it’s clear that most of the time the idea of being broccoli isn’t motivating people to drive past the burger joint instead of through it.
Attempting to inspire better eating habits, nutrition educators have long told people, “You are what you eat,” with the notion that “being” broccoli is more compelling than “being” a double cheeseburger or a supersized beverage. Yet, as we observe the global obesity epidemic and the dietary challenges we see daily with clients, it’s clear that most of the time the idea of being broccoli isn’t motivating people to drive past the burger joint instead of through it.
What’s worse? The axiom “You are what you eat” is actually not true. You are not what you eat, but you are what you digest and absorb. The difference—between eating broccoli and your cells getting nutrients digested from broccoli—is everything when it comes to enabling better health and delivering the results clients seek from their investment in you. With optimal digestion, the body takes in food and turns it into fuel for tasks ranging from improving energy to repairing cells and tissues to identifying and removing waste products. Without optimal digestion, the body struggles to prioritize needs, perhaps passing on repair work in order to enable energy or address a crisis; in short, it works less efficiently and less effectively (Karasov & Douglas 2013).
Today, many adults nationwide experience digestive complaints or diseases (NIH 2009). Statistics reveal staggering numbers of people attempting to manage reflux, constipation, diarrhea, bloating and other symptoms, often without discussing the problems with a physician or healthcare provider. One look at the sales growth of probiotics, laxatives and popular over-the-counter digestive medications points to a nation not digesting or absorbing nutrients well (Johnson 2016).
U.S. Adults Are Digestively Distressed
A quick glance at some key stats strengthens the evidence that digestive health among Americans needs to improve.
- Digestive diseases affect 60–70 million Americans (NIH 2009).
- In 2004, 20% of the population was diagnosed with GERD (gastroesophageal reflux disease) (El-Serag et al. 2004).
- In 2004, 5.9 million prescriptions were written for IBS (irritable bowel syndrome) and 2.1 million for ulcerative colitis (Everhart 2008).
- In 2013, 72% of U.S. adults (men and women) said they had experienced at least one of the following gastrointestinal (GI) symptoms a few times a month or more: diarrhea, gas, bloating, stomach pain, frequent bowel movements, unexplained weight loss or nonspecific GI symptoms. A majority said they had lived with their symptoms for more than 6 months (AbbVie 2013).
Herein lie clues for why, as a country, we are not seeing great headway in our battle with the bulge(s). After all, if one’s digestive system is not working optimally, then it is improbable that metabolism, natural detoxification and elimination efforts are yielding optimal results. To that end, anyone seeking to shed weight, lose fat, gain lean body mass and improve performance must first focus on an assessment of his digestive health.
When Is Digestive Assessment Called For?
If a client eats well (as evidenced by your thorough review of her food journal), and is active (but not getting the body composition results you would expect from her training efforts), consider referring her to a doctor or dietitian for a digestive assessment.
You might also ask a few simple questions to get clues about her digestive health:
- Do you have reflux, or are you bloated after eating normal meals and snacks?
- Are you having difficulty going to the bathroom, or are you not going regularly?
- Are you relying on medications or supplements to help your digestive system work and feel better?
If the client answers yes to any of these questions (or especially to all of them), refer her to a doctor or dietitian for thorough assessment and recommendations.
A 6-Step Tune-Up for Better Digestive Health
Yes, you can have your cake and eat it, too! Improved digestive nutrition enables better health when you make better, not perfect, choices more often. Aiming for perfect will make you perfectly stressed, which will challenge digestion further, and as such be perfectly unhelpful and unhealthy. Here are six suggestions to help clients get optimal digestion and absorption up and running:
-
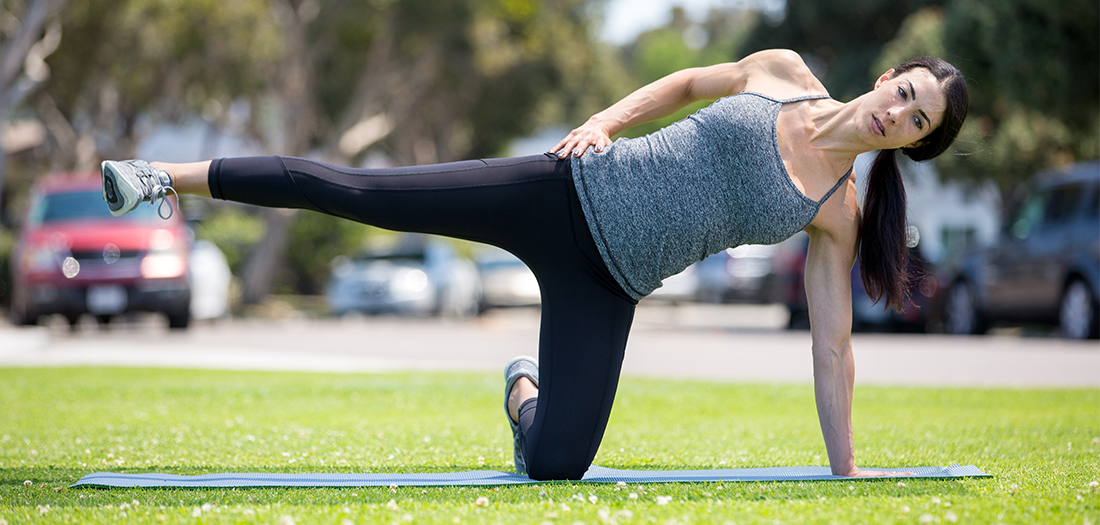
- Move more. The body’s digestive tract is a series of muscles whose ongoing movement enables better digestion. Beyond exercise, it is critical to find opportunities to move throughout the day. Additionally, doing abdominal twists (seated or lying on the floor), as well as bending in all planes of motion, can help to engage and support digestive muscle movement. Work with clients to ensure proper form and to emphasize not just twisting from the shoulders but actually moving the whole core to encourage abdominal muscle movement.
-
- Reduce (digestive) workload. The digestive system can handle a lot, but it can also get overwhelmed. By eating and drinking less at any one time, and by practicing better nutrient balance, clients can give their bodies a manageable workload that allows for efficient, effective work plus time for recovery and relaxation.
-
- Turn off digestive “DiStress.” Certain nutrients and nutrient forms can support the digestive system, reducing stress on it and allowing food to be broken down and absorbedmore efficiently. For example, cacao, nuts, seeds, grains, greens and beans supply your cells with magnesium, which turns off the body’s stress response (“fight or flight”) (Wienecke & Nolden 2016). Avocado,beans, goat’s milk kefir and cheese, raw spinach, and parsley provide glutamine, which helps repair the digestive tract lining, enabling easier and better absorption of nutrients (Rao & Samak 2012).Under stress, the body shunts attention away from digestion, which can make liquid nutrition a great temporary fix for aiding absorption.
Nutrient-balanced liquid-nutrition recommendations include nonstarchy-vegetable-based soups with one serving of starchy vegetable, topped with hemp hearts or chopped nuts; and smoothies with one serving of fruit, nonstarchy vegetables, quality protein powder and a nut butter or other healthy fat.
- Build better balance. Fibers are essential to digestive health. Our bodies need both the insoluble and soluble forms, including those that function as prebiotics (food for probiotics). Bear in mind, however, that too much fiber at once can overwhelm the digestive tract, especially if it is already stressed or irritated. Balance your daily intake by splitting it up throughout the day (aim for 5–10 grams of fiber at one time, versus 20–25 g) and consuming an adequate amount of water daily (as a goal for how many ounces to consume daily, begin with half a client’s body weight in pounds, then split that number into 3–5 water breaks, as a starting point). Balance bacteria load by taking in probiotics from quality fermented foods to counter the “bad” bacteria ingested through our mouths and skin.
- Turn off digestive “DiStress.” Certain nutrients and nutrient forms can support the digestive system, reducing stress on it and allowing food to be broken down and absorbedmore efficiently. For example, cacao, nuts, seeds, grains, greens and beans supply your cells with magnesium, which turns off the body’s stress response (“fight or flight”) (Wienecke & Nolden 2016). Avocado,beans, goat’s milk kefir and cheese, raw spinach, and parsley provide glutamine, which helps repair the digestive tract lining, enabling easier and better absorption of nutrients (Rao & Samak 2012).Under stress, the body shunts attention away from digestion, which can make liquid nutrition a great temporary fix for aiding absorption.
-
- Bite better. Chewing food more thoroughly and chewing on better-quality food give the body more of the resources it needs. Avoid the chemistry lab projects and hyperprocessed foods where nutrients are removed and only some are added back, in different forms, via fortification.
- Journal it. As with anything, we can’t know what’s working and what needs attention without knowing what we are consuming and how our body responds to it most often.
References
AbbVie. 2013. New survey reveals more than half of Americans are living with gastrointestinal symptoms and not seeking care from a doctor. AbbVie press release. Accessed Feb. 1, 2017. https://news.abbvie.com/news/new-survey-reveals-more-than-half-americans-are-living-with-gastrointestinal-symptoms-and-not-seeking-care-from-doctor.htm.
El-Serag, H.B., et al. 2004. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology, 126 (7), 1692–99.
Everhart, J.E. (Ed.). 2008. The Burden of Digestive Diseases in the United States Report. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, NIH Publication 09–6433.
Fahey, J.W., & Stephenson, K.K. 1999. Cancer chemoprotective effects of cruciferous vegetables. Journal of Horticultural Science, 34 (7), 1159–63.
Johnson, C. 2016. Growth of digestive health market and popular ingredients. Natural Products Insider. Accessed Jan. 27, 2016. www.naturalproductsinsider.com/articles/2016/05/growth-of-digestive-health-market-and-popular-ing.aspx.
Karasov, H.W., & Douglas, A.E. 2013. Comparative digestive physiology. Comprehensive Physiology, 3, 741–83.
NIH (National Institutes of Health). 2009. U.S. Department of Health and Human Services. Opportunities and Challenges in Digestive Diseases Research: Recommendations of the National Commission on Digestive Diseases Bethesda, MD: National Institutes of Health, NIH Publication 08–6514.
Rao, R., & Samak, G. 2012. Role of glutamine in protection of intestinal epithelial tight junctions. Journal of Epithelial Biology and Pharmacology, 5 (Suppl. 1-M7), 47–54.
Wienecke, E., & Nolden, C. 2016. Magnesium intake and stress reduction. MMW Fortschritte Der Medizin, 158 (Suppl. 6), 12–16.
















 In nearly 40 years as a fitness educator, I have never been sidelined by a significant injury, in spite of decades of high-impact classes, rigorous weight training, participation in competitive aerobics, and group exercise schedules that sometimes exceeded 25 hours per week. I attribute my longevity in this grueling business to one thing—cross-training all aspects of fitness, including flexibility.
In nearly 40 years as a fitness educator, I have never been sidelined by a significant injury, in spite of decades of high-impact classes, rigorous weight training, participation in competitive aerobics, and group exercise schedules that sometimes exceeded 25 hours per week. I attribute my longevity in this grueling business to one thing—cross-training all aspects of fitness, including flexibility.
